In fetal shunt placement, a shunt (hollow tube) is inserted through the mother’s abdomen and uterus and into the fetus to drain fluid from the amniotic cavity or a fluid-filled anomaly.
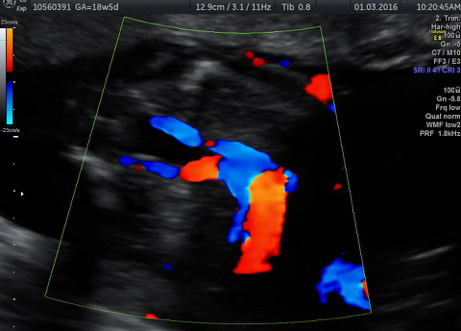
The most common type of fetal shunt placement is pleuro-amniotic shunting for primary hydrothorax to prevent congestive cardiac failure.
The parent is worked up extensively to see whether it is appropriate to shunt the fetus. The ACFM protocal for pleuro-amniotic shunt is as follows
- Diagnostic and therapeutic tap + Amniocentesis
- Samples sent for TLC, DLC, protein, glucose, cytology – ascertain nature of fluid
- Primary hydrothorax
- Review after 1 week, offer shunting at gestational age 18 to 32 weeks if there is
- Rapid refilling
- Unilateral effusion with mediastinal shift
- Bilateral effusion
- Hydrops
The other type of fetal shunt is is vesicoamniotic shunting for urinary tract blockages, such as bladder outlet obstruction. These Lower Urinary Tract Obstructions have a high mortality and high morbidity. the Central pathology is association with cystic renal dysplasia and Abnormal (glomerular and tubular) renal dysfunction. the Underlying pathology -Posterior urethral valves 64% -urethral atresia 39%. Usefulness of this procedure is still under trial.
About the procedure
When a fetus’ urinary tract is blocked completely, the bladder becomes enlarged, and the amount of amniotic fluid decreases (oligohydramnios). This may cause:
- underdeveloped lungs (pulmonary hypoplasia)
- deformities of the face and extremities (Potter sequence)
- kidney damage
A vesicoamniotic shunt creates an alternate way for the urine to bypass the obstruction, allowing the urine to drain into the amniotic cavity and restore normal fluid levels.
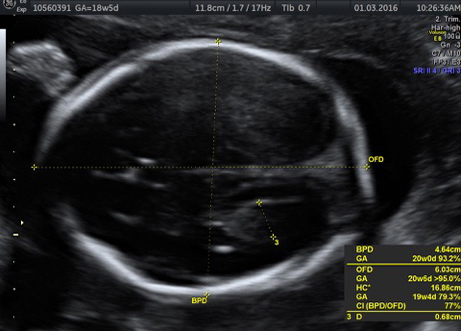
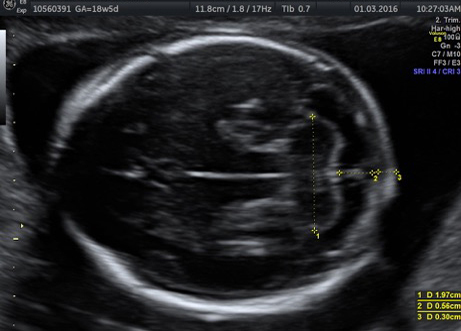
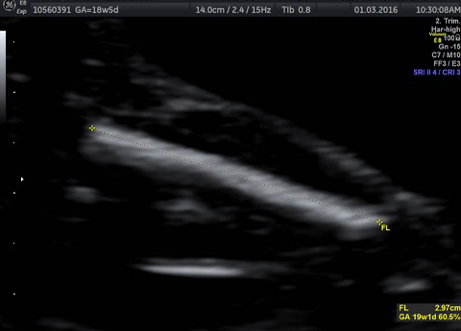
Before considering fetal shunt placement, an extensive evaluation, including ultrasound, fetal MRI, fetal echocardiogram, serial renal function profile and chromosomal analysis, will be conducted. Ideally, the procedure should be performed before the fetus’ lungs and kidneys have fully developed.
The procedure is performed in the hospital on an outpatient basis. The mother is given ID sedation, which also sedates the fetus, as well as antibiotics and local anesthesia. Using ultrasound guidance, a metal cannula (tube) on a trochar needle is placed through the mother’s abdomen and uterus, then into the fetus’ bladder. The trochar is removed, and a drainage catheter is inserted into the cannula, with one end of the catheter in the bladder and the other in the amniotic cavity. The cannula is removed, and correct placement is confirmed by ultrasound.
Amnioinfusion, a surgical procedure that adds fluid to the amniotic sac, may be needed as well.
Side effects of fetal shunting may include premature labor, trauma to the fetus, chorioamniotic separation and intraplacental bleeding.
Outcomes are determined by the cause and severity of the problem, as well as any co-existing conditions. The mother and fetus will be monitored closely for the remainder of the pregnancy.