Intrauterine transfusion is a procedure in which red blood cells from a donor are injected into the fetus.
Intrauterine transfusion may be recommended when a fetus has anemia (low red blood cell count). Fetal anemia may be caused by:
- Rh incompatibility: When the mother and fetus have different blood types, the antibodies in the mother’s blood may destroy blood cells in the fetus
- Parvovirus B19 viral infection in the mother
Goals of intrauterine transfusion are to prevent or treat fetal heart failure (hydrops), which can be caused by anemia, and to allow the pregnancy to continue so the baby can be more developed when it is born.
Once the decision to transfuse is taken, then a O negative donor needs to be arranged by the family. The donor should not be a diabetic, use alcohol, have jaundice or have recently given blood.
The blood then is tested for haemoglobin, blood group, cross matching, atypical antibodies and screened for infection such as for HIV, HCB, HBB, HBcAb, VDRL and Malaria. This takes 6-8 hours and then a nucleic acid testing for HIV, HB and HC is again done. This takes another 5 hours. The blood is then hemo-concentrated such that the hematocrit is about 80%. It is then irradiated and is ready for intrauterine transfusion.
There are two methods to perform fetal blood transfusions. In both, a needle is inserted into the mother’s abdomen.
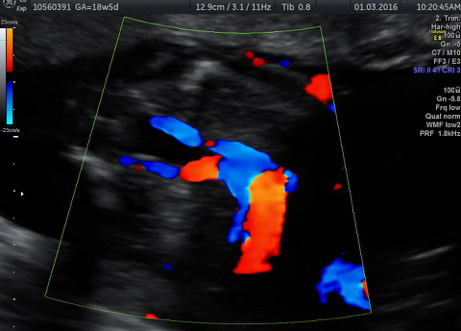
- Intravascular transfusion (IVT): blood is transfused into the umbilical cord
- Intraperitoneal transfusion (IPT): blood is transfused into the fetus’ abdomen.
This is not as common.
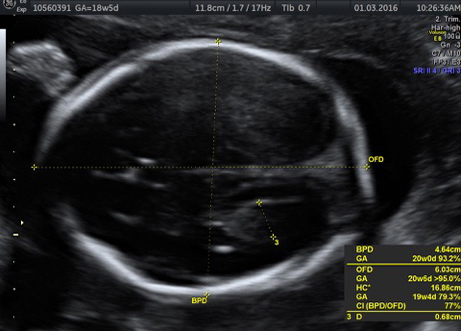
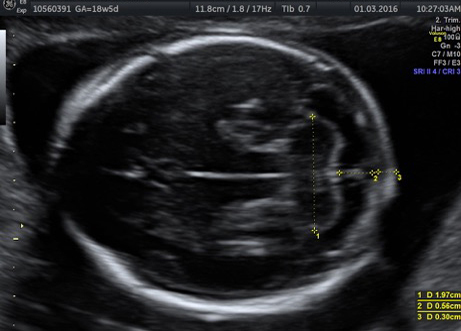
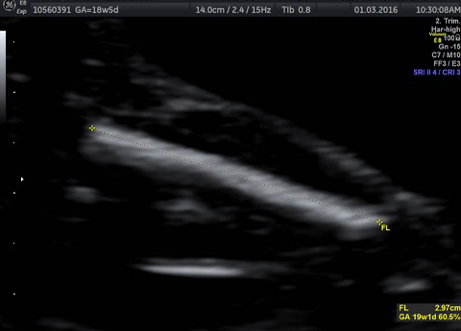
Intrauterine transfusion is performed in the hospital, usually on an outpatient basis. You will be given antibiotics and local anesthesia. The fetus may be given additional medicine to stop movement. Using ultrasound to determine the position of the fetus and placenta, the surgeon inserts a needle into your abdomen and then into the umbilical cord vein. Red blood cells that are compatible with the fetus’ blood type are passed through the needle into the fetus. The doctor will prescribe antibiotics and medication to prevent labor. Fetal transfusions may need to be repeated every few weeks until the fetus is ready to be born.
The chance of problems is rare, but there are risks in every procedure. In intrauterine transfusion, these may include:
- Fetal distress and the need for cesarean section delivery if transfusion is taking place at greater than 28 weeks
- Premature labor
- Cramping or vaginal bleeding or discharge
- Infection
During your evaluation, we will provide a detailed review of your baby’s condition and treatment options in order to help you and your family decide what the best treatment plan may be.