“We’ll help you prepare for multiple blessings”
Our unique Twin Pregnancy Clinic offers you personalized services if you’re pregnant with 2 or more babies
Knowing you’re having more than one baby can be exciting and overwhelming at the same time. We’re as concerned as you are about your health and the health of your babies. That’s why our Twin Pregnancy Clinic offers you genetic counseling, fetal imaging and nutritional guidance during the most crucial time of development.
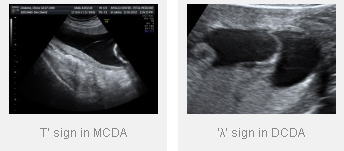
When two sperms fertilize two eggs, two embryos are formed who have their own placentas (afterbirth). These non-identical or ‘fraternal’ twins constitute 80% of twin pregnancies and are called dichorionic diamniotic (DCDA) twins. When one sperm fertilizes an egg which divides into two later on, identical twins or monochorionic twins are formed. These are the rarer variety where the twins are of the same sex, have the same genetic makeup and share the same placenta.
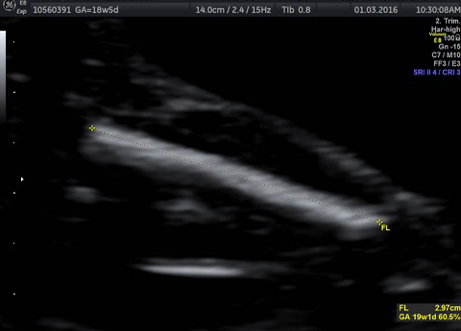
The diagnosis of twin pregnancy is confirmed on ultrasound.
The mother may have more pronounced minor side effects of pregnancy like morning sickness, abdominal heaviness, mechanical difficulties due to the larger size of the womb, more swelling of the feet etc.
More frequent hospital visits and more frequent ultrasound scans
An expectant mother with twin pregnancy would need more frequent hospital visits and more frequent checkups than their singlet on counter parts.
Most twin pregnancies will have an uneventful course and normal delivery; however it is important to be aware of the following complications:
Anaemia
Since there is increased demand for nutrients for two babies rather than one, there is increased risk of developing anemia and other nutritional deficiencies.
High blood pressure
Mothers with multiple pregnancy have a higher chance of developing high blood pressure in pregnancy.
Premature delivery
Since the womb is getting over distended with more babies than one, almost 50% twins will deliver earlier than 37 weeks and have lower birth weights than an average singleton. Almost one in ten will deliver before 32 weeks of pregnancy.
Operative delivery
There is a higher chance of instrumental vaginal delivery or caesarean delivery in twin pregnancy.
Dichorionic or non-identical twins:
There is a high chance of preterm delivery, growth restriction and low birth weight (<2.5 kg) in twin pregnancy. Preterm infants are at risk of lung immaturity, infection, intestinal problems and require prolonged hospital stay.
Monochorionic or identical twins:
 In addition to above risks, there is a small increased risk of birth defects in identical twins. They are also at risk of complications arising from unequal sharing of the placenta which include differential growth patterns, twin twin transfusion syndrome (TTTS), acardiac twinning and even death of a single baby leading to neurological complications in the surviving twin.
In addition to above risks, there is a small increased risk of birth defects in identical twins. They are also at risk of complications arising from unequal sharing of the placenta which include differential growth patterns, twin twin transfusion syndrome (TTTS), acardiac twinning and even death of a single baby leading to neurological complications in the surviving twin.
Yes, a mother with twin pregnancy needs more specialised care and intensive monitoring for ensuring both maternal and fetal well being and for early detection of complications. This would mean more frequent hospital visits, more investigations and more frequent ultrasound scans. An obstetrician experienced in managing high risk pregnancy and Fetal Medicine specialist should be involved in the care of these mothers. You should deliver in a tertiary care hospital with neonatal intensive care (NICU) facilities.
First trimester screening
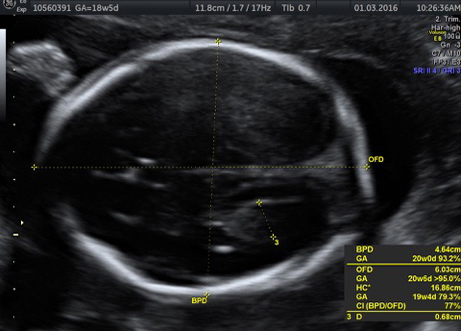
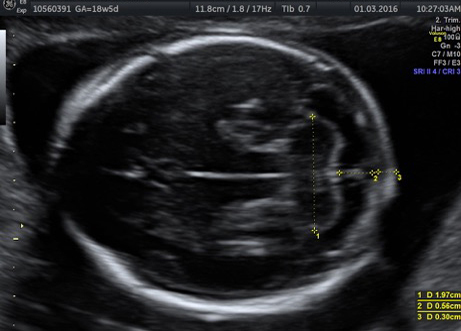
All twin pregnancies should first be seen at around 12 weeks. An ultrasound at this time helps in assigning the ‘chorionicity’which is the single most important factor in determining prognosis and directing further management. At the same time, this scan helps in detection of chromosomal abnormalities like Down syndrome and certain other birth defects in either of the twin.
A fetal anomaly scan is done at 18 to 20 weeks to detect structural abnormalities in either baby. At each visit, the mother’s blood pressure is checked and urine tested for proteins.
Dichorionic (DCDA) twin pregnancy
Further growth scans or fetal well being scans are done at four weekly intervals, ie approximately at 24, 28, 32 and 36 weeks respectively.
Monochorionic (MCDA) twin pregnancy
Monochorionic pregnancies are followed at 2 weekly intervals, ie at 16, 18, 20, 22, 24, 26, 28, 32, 34 and 36 weeks.
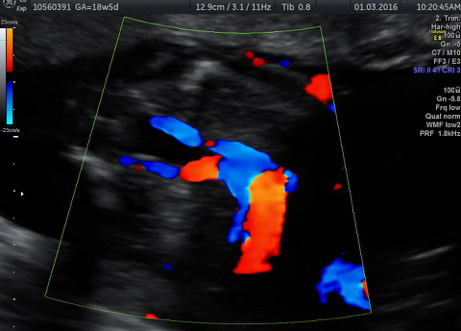
TTTS complicates about 1 in 5 of all monochorionic, ie identical twin pregnancies. It is a very serious condition which endangers the lives of both twins and if untreated, the risk of the fetus dying is as high as 90%
Unfortunately there are no preventive strategies for TTTS. It is a complication which is unique to this particular type of twins. Hence, it is very important to know the ‘type’ of twin pregnancy making an early ultrasound in the third month of pregnancy essential. We can detect TTTS early by doing regular ultrasounds.
How is it treated?


The best treatment available for TTTS is ‘LASER ablation’. Simply put, a Laser beam is used to destroy the abnormal vascular connections connecting the two twins. It is performed by a Fetal Medicine expert and is done under local anaesthesia.
The procedure is done in theatre and usually takes about 30 to 60 minutes. A 2-3 mm telescope is inserted into the amniotic cavity through a minute incision on the mother’s tummy. The abnormal vessels are then burnt under direct vision. In addition, the excessive liquor may be drained from the recipient twin’s sac at the same time. You will be kept under observation for some time in the hospital and will be discharged the next day.
The other option is serial amniodrainage
this means repeated drainage of increasing amount of amniotic fluid from the recipient twin’s sac. However the outcome has been proved to be much inferior to Laser ablation and it is done only when the former is not available.
Selective fetal reduction in discordant anomalies
In case one of the twins has an abnormality and the other twin is normal, one of the twins is ‘reduced’for the sake of the normal twin.
Cord coagulation for MCDA twins
Interstitial Laser coagulation for TRAP
* Accredited by Fetal Medicine Foundation, UK