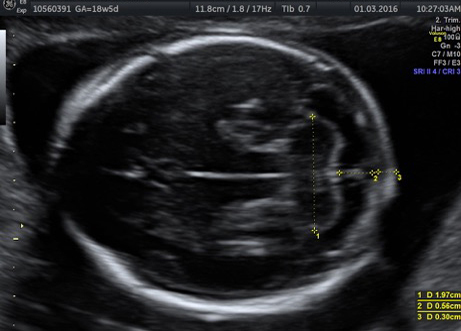
Hypoplastic left heart syndrome is a condition that occurs in approximately 1 in 6,000 live births where the fetus’ left ventricle, mitral valve and aortic valve are severely under-developed. As less blood crosses the mitral and aortic valves, the left heart stops growing. By time of birth, the left ventricle is too small to function to pump blood out of the heart.
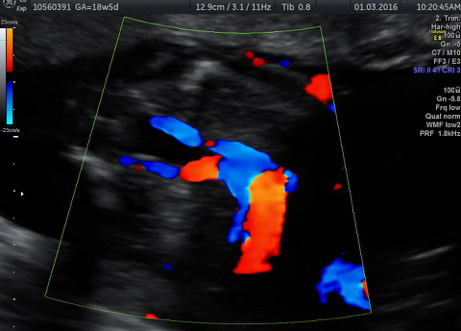
Due to the inability of blue blood (deoxygenated) and red blood (oxygenated) to mix when the atrial septal defect is very small or absent in HLHS, the majority of blood pumped to the baby’s body is lacking oxygen, resulting in a blue cyanotic skin discoloration and rapid deterioration of the baby. When there is an atrial septal defect in HLHS, the red blood can pass from the left atrium into the rest of the heart and result in a much more stable, less cyanotic baby.
In fetuses with HLHS, it is also critical that there is an open communication between the atrial chambers, otherwise flow returning from the lungs becomes severely obstructed. The resulting pulmonary hypertension and lung damage causes the infant to be markedly unstable after delivery, requiring urgent cardiac catheterization. Often these infants are not candidates for cardiac repair and die.
If a fetus is determined to have hypoplastic left heart syndrome (HLHS) with an intact atrial septum, they may be a candidate for a balloon atrial septostomy.