Because one half of a fetus’s genetic makeup comes from the father, it is possible for a fetus to have a different type of platelets from the mother. In rare cases, the mother’s defensive cells do not recognize the fetus’s platelet type and make proteins called antibodies that can cross the placenta and fight against a fetus’s platelets. When this occurs, the result can be fetal thrombocytopenia, or low platelets, due to platelet alloimmunization, and the fetus may have episodes of internal bleeding. This condition is usually diagnosed after delivery, due to low platelets or bleeding noted in a newborn.
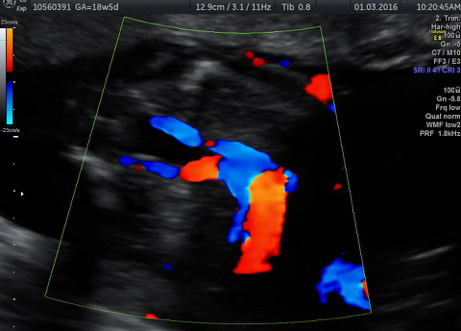
Once a pregnancy is affected by this condition, there is a high likelihood of future pregnancies being affected even more severely. Testing of the parents and fetus is undertaken, and if the fetus is considered to be at high risk for platelet alloimmunization, treatment may be offered to decrease the risk of internal bleeding. This treatment may include intravenous antibodies (IVIG), steroids and/or platelet transfusions directly into the fetal umbilical cord while the fetus is still in the uterus. This procedure can be somewhat risky but also life-saving. Treatment will continue for the length of the pregnancy. After delivery of the baby, additional treatment with medication or platelet transfusion is often necessary.