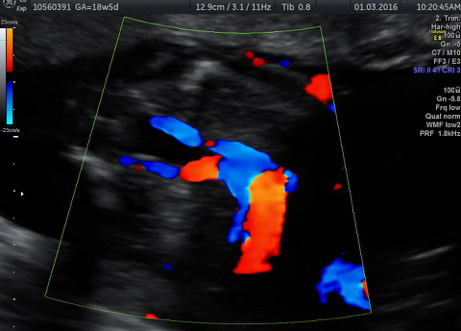
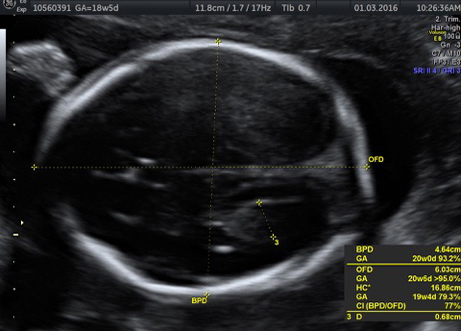
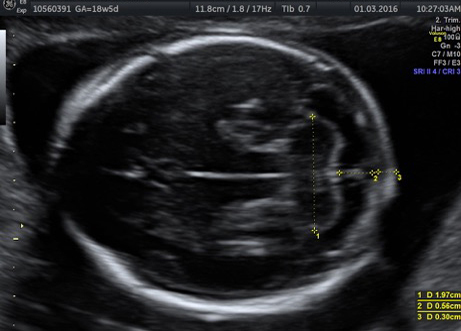
Because one half of a fetus’s genetic makeup comes from the father, it is possible for a fetus to have a different blood type from the mother. In rare cases, because of previous exposure to a blood transfusion or blood cells from a prior pregnancy, the mother makes defensive proteins called antibodies that can cross the placenta and fight against a fetus’s blood cells. This process, called red cell alloimmunization, can cause severe fetal anemia and even death if not monitored and treated. When routine testing shows that a mother has antibodies, more specialized testing can be done of the father and the fetus, and ultrasound monitoring may be necessary to check the fetus for anemia.
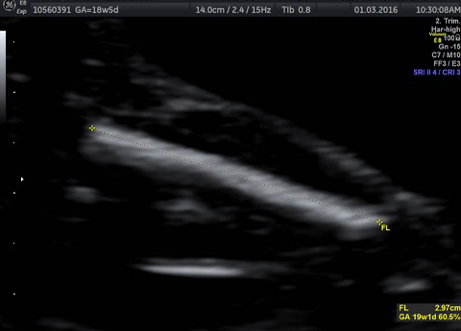
If anemia is detected in the fetus, a blood transfusion can be performed to replace the fetus’s blood supply. The transfusion is administered through the umbilical cord and/or in the fetus’s belly while the fetus is still in the uterus, as early as 18 weeks of pregnancy. This procedure can be somewhat risky but also life-saving. It often needs to be repeated several times through the pregnancy if subsequent testing shows that the fetus is anemic. After delivery of the baby, another blood transfusion is usually necessary.
Once a pregnancy is affected by this condition, there is a high likelihood of future pregnancies being affected even more severely, and close surveillance should be pursued.