Sacrococcygeal Teratoma (SCT) is a tumor, or growth, on the coccyx (tailbone). It is the most common type of tumor in newborns, occurring in one in 35,000 births. SCT is found more often in girls than boys.
Prenatal SCTs can be internal (growing inside the fetus’ body) or external (growing out of the body). Usually, they are small and benign (non-cancerous) and cause no problems during pregnancy. However, they can grow large — in some instances larger than the fetus.
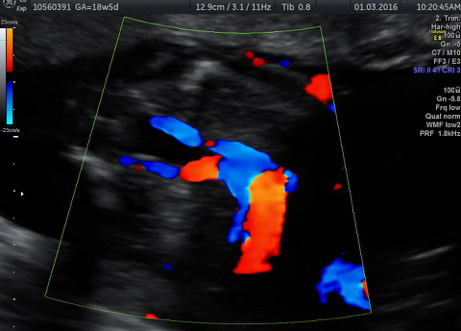
SCTs can develop large blood vessels that make the fetus’ heart work harder to pump blood to the tumor and the rest of the body. This can cause overproduction of amniotic fluid and fluid retention, which can prompt heart failure, also called hydrops. This dangerous condition can develop rapidly, and it is often fatal for fetuses fewer than 30 weeks gestation.
In rare cases, the mother may develop a “maternal mirror” syndrome in which her condition is similar to, or “mirrors,” that of the fetus.
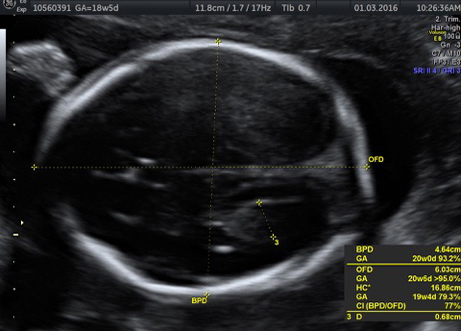
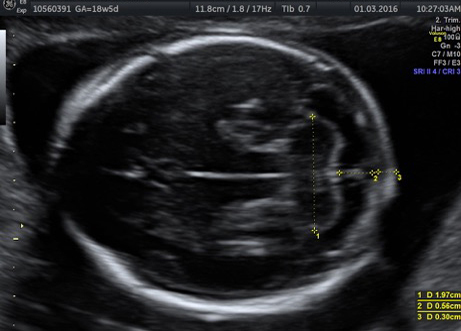
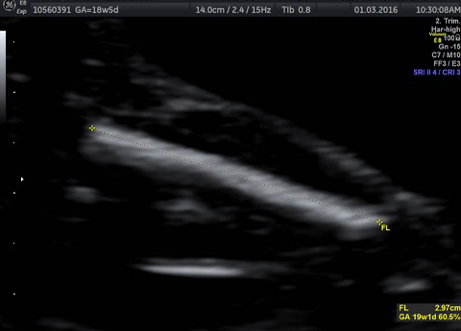
External SCTs may be found during routine prenatal ultrasounds. Usually, however, a routine prenatal blood test shows a high level of alpha-fetoprotein (AFP) in the mother’s blood, leading to an ultrasound that shows the tumor. Sometimes the uterus is larger than it should be, which may be caused by high levels of amniotic fluid or a large tumor.
If SCT is suspected, a specialized ultrasound will be performed. The mother will be monitored closely throughout the pregnancy, and further ultrasounds, as well as fetal echocardiogram, will be performed. If the SCT is large, a cesarean delivery may be recommended.
The treatment for SCT depends on the tumor size and location. Usually, the SCT is surgically removed and perineum repaired within a few days after birth. If hydrops develops late in pregnancy, a planned cesarean may be necessary. If the SCT develops earlier in pregnancy, the mass may be removed by open fetal surgery or radio-frequency ablation.
After removal, the tumor will be biopsied to determine if it is malignant (cancerous) or benign.
If an SCT is present, it’s important for the mother to deliver the baby at a hospital with a multidisciplinary team and a high-level neonatal intensive care unit.