We are only unit in north India who are accredited to perform the First Trimester Down Syndrome Screening according to the standards laid down by the Fetal Medicine Foundation UK. This screening involves an ultrasound assessment of the fetus including the nuchal translucency, and the new markers such as nasal bone, tricuspid regurgitation and ductus venosus PI.
The maternal blood is also checked for PAPPA, free beta- HCG and PLGF and an integrated risk assessment is given.
The First Trimester Screening (FTS) test has important implications for you and your family and we have explained here how it is performed and what the results mean. Before undergoing this test it is very important that you have discussed this testing procedure.
Tests which tell if your baby has a particular disease or condition with certainty are called diagnostic tests. On the other hand, screening tests only show if your baby’s chance is high or low for a specific disease or condition. If the chance is increased, you can then choose to have a diagnostic testing.
The vast majority of babies are normal. However all women, whatever their age, have a small risk of delivering a baby with a physical or a mental abnormality. In some cases this may be due to chromosomal problems such as Down syndrome, Trisomy 13 or Trisomy 18. These conditions are mainly looked for in the first trimester screening.
Chromosomes contain the genetic information we require to grow and develop normally. Each cell contains 23 pairs of chromosomes. Down syndrome usually occurs by having 3 copies of chromosome 21. It occurs in about 1 in every 700 pregnancies and is an important cause of congenital intellectual disability. It causes intellectual disability and various medical problems involving the heart, digestive tract, and/or other organ systems.
Trisomy 18 (having an extra chromosome #18) and trisomy 13 (having an extra chromosome #13) are more severe disorders which cause profound mental retardation and severe birth defects in many organ systems. Few babies with trisomies 13 or 18 survive more than a few months.
What causes this replication is still unknown, no racial, geographical, social, economic or environmental factors have been identified.Anyone can have a baby with these chromosome abnormalities, however, the chance increases with the mother’s age, but a child with Down Syndrome can be born to a mother of any age.
Leading medical professional organizations recommend first trimester Down syndrome screening for all pregnant women, regardless of age.
First trimester screening is not a diagnostic test, which means it cannot tell you whether your baby has Down syndrome, trisomy 13, or trisomy 18. Instead, the screening provides a probability that your baby might have Down syndrome, trisomy 13, or trisomy 18.
This probability or chance is based on the following criteria:
- Your age
- Nuchal Translucency (amount of fluid behind the neck of the fetus on ultrasound)
- Presence or absence of any physical abnormalities on ultrasound
- Level of three proteins (Fß-hCG, PAPP-A and PLGF) in your blood.
The screening results can either alert you and your doctor that your baby is at an increased risk for one of these chromosome disorders or be reassuring that your baby is at a lower risk for these conditions.
Women at high risk are offered further tests. It is important to remember that most women will have normal babies, even if they are grouped as high risk.
It involves two tests, a blood test and an ultrasound.
Blood Test – We recommend women have the blood test at week 10 of pregnancy. However, the blood test can be performed up until 13 weeks and 6 days of pregnancy. It analyzes three chemicals called free beta-human chorionic gonadotropin (hCG) , pregnancy associated plasma protein-A (PAPP-A), and placental growth factor (PLGF) which are found in the blood of all pregnant women.
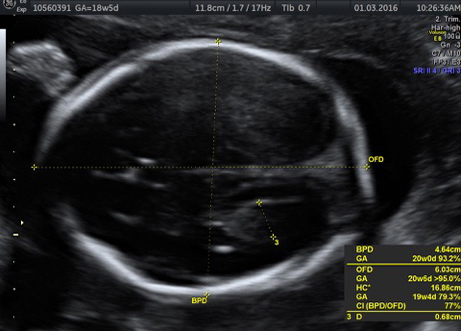
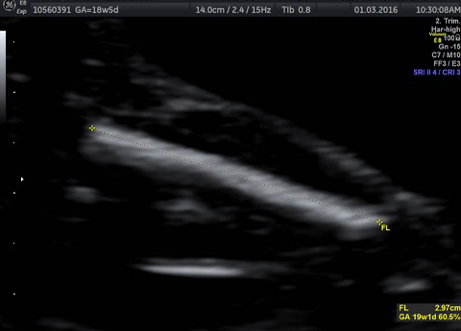
Ultrasound – We recommend the ultrasound is performed at week 12 of pregnancy. However, the ultrasound can be performed from 11 weeks through to 13 weeks and 6 days of pregnancy. It is a highly specialized ultrasound. It takes about 30-40 minutes.
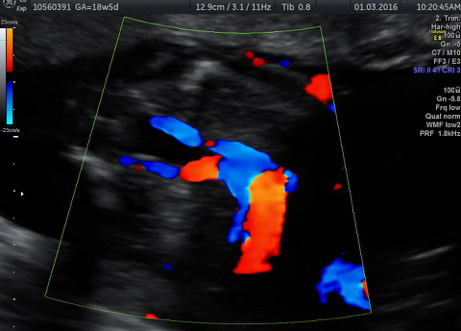
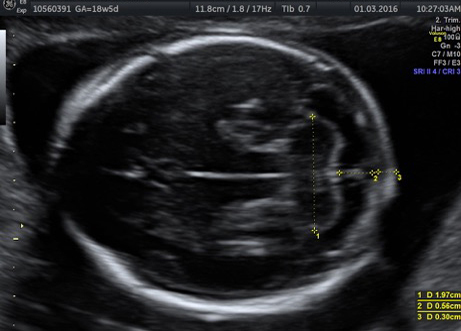
The sonogram will confirm how far along your pregnancy is. In addition, a measurement of the fluid underneath the skin along the back of the baby’s neck, called the nuchal translucency (NT), will be taken. The sonogram will also determine if your baby’s nasal bone is present or absent. It will also check the blood flow across the valve of the right heart chamber and look for regurgitation ( tricuspid regurgitation) and blood across the ductus venosus, the physiological valve regulating blood to the heart.
Combining your age-related risk with the NT measurement, nasal bone data, and blood work, provides you with one risk figure for Down syndrome and one risk figure for trisomy 13 or trisomy 18.
This special scan also provides other very useful information:
- Accurate dating of the pregnancy
- Fetal heart rate
- Number of fetuses present and, if twins, whether they are identical or not
- Detects obvious fetal abnormalities
Except for the discomfort of drawing blood, there are no known risks or side effects associated with the First trimester screen.
Because this is a screening test, a positive result (showing an increased risk) does not mean that your baby has a problem, only that further diagnostic tests are options for you to consider. Also, a negative or normal result (one that shows a decreased risk) does not mean that the baby will not have a chromosome abnormality.
The first trimester screen’s detection rate is approximately 96% for pregnancies in which the baby has Down syndrome, and is somewhat higher for pregnancies with trisomy 13 or trisomy 18. There is a 5% false positive rate for the test. Parents should be aware of the possibility of receiving abnormal results and then finding, after further testing, that the baby is normal. In our unit, we take a cutoff of T21 at 1:250 thus the results are either screened +ve or _ve.
Finally, this screen is not designed to provide information about the possibility of other chromosome conditions, nor about many other genetic syndromes, genetic disorders, birth defects, or causes of intellectual disability.
What does a “screen negative” result mean?
Screen negative means that the probability that your baby has Down syndrome is better than 1:250
It is important to remember that a screening test does not guarantee a normal baby.
If your First Trimester Screen is “screen negative”, your obstetrician will provide you with routine obstetrical care.
What does a “screen positive” result mean?
A screen positive result means that there is an increased risk for Down syndrome, trisomy 13, or trisomy 18 in the pregnancy. A screen positive result does not mean that the fetus is affected with the condition, only that a pregnancy has an increased risk for the condition. Most women with “screen positive” results have healthy babies.
When the result is “screen positive”, the following options are available:
- Diagnostic testing by chorionic villus sampling (CVS) performed between 10-13 weeks
- Diagnostic testing by amniocentesis performed after 15 weeks
- Second trimester maternal serum screening drawn after 15 weeks to obtain a combined first and second trimester screening result
- Detailed anatomy ultrasound performed at approximately 18-20 weeks
What are the diagnostic tests available?
Diagnostic tests will usually involve amniocentesis or chorionic villus sampling, which take a small amount of fluid or tissue from around the baby for chromosomal analysis.
Both tests have a small risk of miscarriage.
CVS and amniocentesis are diagnostic tests that can tell you with greater than 99% accuracy whether or not a baby has a chromosome abnormality.
Final results from the chromosomal analysis may take 2-3 weeks. Usually an interim result may be available in a few days. We will discuss the results with you and assist you in deciding about diagnostic tests, such as CVS or amniocentesis.
The reasons to pursue further testing or not vary from person to person and couple to couple. Performing further testing allows you to confirm a diagnosis and then provides you with certain opportunities:
- Pursue potential interventions that may exist (i.e. TRAP or laser for acardiac twins)
- Begin planning for a child with special needs
- Start addressing anticipated lifestyle changes
- Identify support groups and resources
- Make a decision about carrying the child to term
Some individuals or couples may elect not to pursue testing or additional testing for various reasons:
- They are comfortable with the results no matter what the outcome
- Because of personal, moral, or religious reasons, making a decision about carrying the child to term is not an option
- Some parents choose not to allow any testing that poses any risk of harming the developing baby
It is important to discuss the risks and benefits of testing thoroughly. We will help you evaluate if the benefits from the results could outweigh any risks from the procedure.